

Medicine, surgery,ophthalmology,psychiatry,dermatology,ENT disease,treatment,cure,diagnosis,complications, Medical cases Ebooks free downloads medical videos Gallery


is the most common Cyanotic heart disease in children. The condition causes mixing of deoxygenated blood with the oxygenated blood being pumped out of the heart and into the circulatory system of blood vessels, Causing-
Because rickets results from a metabolic disturbance, the underlying disease should be diagnosed. The causes of rickets can be classified into 11 main categories:

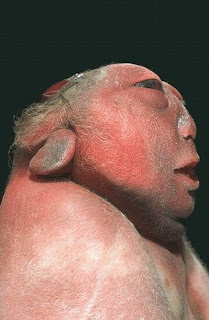
 Apert Syndrome
Apert Syndrome


Apert syndrome is a rare genetic disorder that is characterized by specific craniofacial and limb abnormalities. It is caused by a genetic mutation in the FGFR2 gene on chromosome 10. The mutation can be inherited from a parent who has Apert syndrome or it can be a spontaneous (new) mutation. Studies show that Apert syndrome tends to occur more often in children with older fathers. Furthermore, all new mutations (those that have not been inherited by an affected parent) have been shown to occur exclusively in the FGFR2 gene received by the father. Apert syndrome occurs in 1 out of 100,000 to 160,000 live births and affects males and females equally. The first reported case of the syndrome was in 1848 by S.W. Wheaton, and in 1906, a French physician named E. Apert described nine cases and defined the syndrome.
Features and Characteristics
The following characteristics have been found in children with Apert syndrome:
| Hyperhidrosis Synonychia Brittle nails Severe acne in puberty Interruption of the eyebrows Hypopigmentation Hyperkeratosis Paronychial infections of plantar skin Excessive skin wrinkling of forehead Dimples at knuckles, shoulders and elbows |
Prematurely Fused Cranial Sutures
Retruded Mid-face
Fused Fingers and Toes
Diagnosis
The diagnosis can be made by a skull x-ray, which will confirm premature closure of the skull, and by a clinical exam. The combination of the craniofacial problems and the fused fingers and toes is what distinguishes Apert syndrome from other similar syndromes. Since the defect which causes Apert syndrome has been identified, genetic testing can be provided to confirm a diagnosis.
Treatment
Treating a child with Apert syndrome is best accomplished with a team approach. This would include a craniofacial surgeon, neurosurgeon, ENT specialist, audiologist, speech pathologist, oral surgeon, psychologist, ophthalmologist, and an orthodontist. The majority of treatment methods is surgical and the individual will likely require many operations. Aside from the surgeries required to correct the craniofacial problems and the fused fingers and toes, there may be other potential surgeries to improve the upper airway, address severe eye problems, or correct dental issues.
 co
co ordinating area of the brain). The remaining brain tissue is often exposed--not covered by bone or skin. The infant is usually blind, deaf, unconscious, and unable to feel pain. Although some individuals
ordinating area of the brain). The remaining brain tissue is often exposed--not covered by bone or skin. The infant is usually blind, deaf, unconscious, and unable to feel pain. Although some individuals  with anencephaly may be born with a rudimentary brain stem, the lack of a functioning cerebrum permanently rules out the possibility of ever gaining consciousness. Reflex actions such as respiration (breathing) and responses to sound or touch may occur. The cause of anencephaly is unknown. Although it is believed that the mother's diet and vitamin intake may play a role, scientists believe that many other factors are also involved.
with anencephaly may be born with a rudimentary brain stem, the lack of a functioning cerebrum permanently rules out the possibility of ever gaining consciousness. Reflex actions such as respiration (breathing) and responses to sound or touch may occur. The cause of anencephaly is unknown. Although it is believed that the mother's diet and vitamin intake may play a role, scientists believe that many other factors are also involved.