Medicine, surgery,ophthalmology,psychiatry,dermatology,ENT disease,treatment,cure,diagnosis,complications, Medical cases Ebooks free downloads medical videos Gallery
Headache : Most common causes
* Common cold
* Flu
* Fever - headaches are common with fever from any type of infection
* Ear infection
* Tooth infection (type of Dental conditions)
* Sinus infection
* Pneumonia
* Measles
* Mumps
* Tonsillitis
* Sinus blockage
* Coughing - too much coughing can cause a form of traction headache.
# Various possible types of headache:
* Migraine
* Cluster headache
* Tension headache
* See also types of headache
# Lifestyle causes
* Hangover
* Excessive alcohol
* Stress
* Fatigue
* Tension
* Tiredness
* Excessive smoking
# Dyspepsia
# Eye conditions
* Glaucoma
* Eyestrain
# Medical procedures
* Spinal tap treatment
* Epidural - this anaesthetic procedure (common for childbirth) can occasionally cause damage to the spinal area and cause headache.
# Systemic or metabolic conditions
* Hypertension
* Thyroid disease
* Anemia
* Kidney failure (type of Kidney disease)
* Uremia
* Lead poisoning - African Folk Remedies - Kohl - headache
* Various toxins - see toxin causes of headache
# Brain or head conditions
* Meningitis
* Encephalitis
* Head injury
* Brain injury
* Mild traumatic brain injury
* Concussion
* Temporal arteritis
* Heatstroke
* Sunstroke
* Blood clots - in the brain, these can cause a stroke.
* Brain aneurysm
* Subdural hematoma
* Stroke
* Transient ischemic attacks
* Subarachnoid hemorrhage
* Brain tumor
* Benign intracranial hypertension
* Trigeminal neuralgia
Malaria : Epidemiology, signs and symptoms
- Malaria is a life-threatening disease caused by parasites that are transmitted to people through the bites of infected mosquitoes.
- A child dies of malaria every 30 seconds.
- There were 247 million cases of malaria in 2006, causing nearly one million deaths, mostly among African children.
- Malaria is preventable and curable.
- Approximately half of the world's population is at risk of malaria, particularly those living in lower-income countries.
- Travellers from malaria-free areas to disease "hot spots" are especially vulnerable to the disease.Malaria takes an economic toll - cutting economic growth rates by as much as 1.3% in countries with high disease rates.


Malaria is caused by parasites of the species Plasmodium. The parasites are spread to people through the bites of infected mosquitoes.
There are four types of human malaria:
Plasmodium falciparum
Plasmodium vivax
Plasmodium malariae
Plasmodium ovale.
Plasmodium falciparum and Plasmodium vivax are the most common. Plasmodium falciparum is the most deadly.
Common symptoms of malaria
In the early stages, malaria symptoms are sometimes similar to those of many other infections caused by bacteria, viruses, or parasites. Symptoms may include:
Fever.
Chills.
Headache.
Sweats.
Fatigue.
Nausea and vomiting.
Other common symptoms of malaria include:
Dry (nonproductive) cough.
Muscle and/or back pain.
Enlarged Spleen
Complications of Malaria( Falciparum):
Cerebral malaria
Algid Malaria
ARDS
Convulsion
Coma
Acute Renal Failure
Hypoglycemia
hyperthermia
hyperparasitemia
severe anemia
Symptomatic diagnosis
Using Giemsa-stained blood smears from children in Malawi, one study showed that when clinical predictors (rectal temperature, nailbed pallor, and splenomegaly) were used as treatment indications, rather than using only a history of subjective fevers, a correct diagnosis increased from 21% to 41% of cases and unnecessary treatment for malaria was significantly decreased.
Microscopic examination of blood films
Field tests
In areas where microscopy is not available, or where laboratory staff are not experienced at malaria diagnosis, there are antigen detection tests that require only a drop of blood. Immunochromatographic tests (also called: Malaria Rapid Diagnostic Tests, Antigen-Capture Assay or "Dipsticks") have been developed, distributed and fieldtested. These tests use finger-stick or venous blood, the completed test takes a total of 15–20 minutes, and a laboratory is not needed. The threshold of detection by these rapid diagnostic tests is in the range of 100 parasites/µl of blood compared to 5 by thick film microscopy. The first rapid diagnostic tests were using P. falciparum glutamate dehydrogenase as antigen.[42] PGluDH was soon replaced by P.falciparum lactate dehydrogenase, a 33 kDa oxidoreductase [EC 1.1.1.27]. It is the last enzyme of the glycolytic pathway, essential for ATP generation and one of the most abundant enzymes expressed by P.falciparum. PLDH does not persist in the blood but clears about the same time as the parasites following successful treatment. The lack of antigen persistence after treatment makes the pLDH test useful in predicting treatment failure. In this respect, pLDH is similar to pGluDH. The OptiMAL-IT assay can distinguish between P. falciparum and P. vivax because of antigenic differences between their pLDH isoenzymes. OptiMAL-IT will reliably detect falciparum down to 0.01% parasitemia and non-falciparum down to 0.1%. Paracheck-Pf will detect parasitemias down to 0.002% but will not distinguish between falciparum and non-falciparum malaria. Parasite nucleic acids are detected using polymerase chain reaction. This technique is more accurate than microscopy. However, it is expensive, and requires a specialized laboratory. Moreover, levels of parasitemia are not necessarily correlative with the progression of disease, particularly when the parasite is able to adhere to blood vessel walls. Therefore more sensitive, low-tech diagnosis tools need to be developed in order to detect low levels of parasitaemia in the field. Areas that cannot afford even simple laboratory diagnostic tests often use only a history of subjective fever as the indication to treat for malaria. Using Giemsa-stained blood smears from children in Malawi, one study showed that unnecessary treatment for malaria was significantly decreased when clinical predictors (rectal temperature, nailbed pallor, and splenomegaly) were used as treatment indications, rather than the current national policy of using only a history of subjective fevers (sensitivity increased from 21% to 41%).
Molecular methods
Molecular methods are available in some clinical laboratories and rapid real-time assays (for example, QT-NASBA based on the polymerase chain reaction) are being developed with the hope of being able to deploy them in endemic areas.
Rapid antigen tests
OptiMAL-IT will reliably detect falciparum down to 0.01% parasitemia and non-falciparum down to 0.1%. Paracheck-Pf will detect parasitemias down to 0.002% but will not distinguish between falciparum and non-falciparum malaria. Parasite nucleic acids are detected using polymerase chain reaction. This technique is more accurate than microscopy. However, it is expensive, and requires a specialized laboratory. Moreover, levels of parasitemia are not necessarily correlative with the progression of disease, particularly when the parasite is able to adhere to blood vessel walls. Therefore more sensitive, low-tech diagnosis tools need to be developed in order to detect low levels of parasitaemia in the field.
Tropical diseases in Asia
Cholera
Dysentery
Intestinal Worms
Dengue Fever
Yellow Fever
Schistosomiasis
Leprosy
Filariasis
Trypanosomiasis
Hepatitis
Chlamydia Trachomatis
Classification: Pneumonia
Early classification schemes
Initial descriptions of pneumonia focused on the anatomic or pathologic appearance of the lung, either by direct inspection at autopsy or by its appearance under a microscope.
A lobar pneumonia is an infection that only involves a single lobe, or section, of a lung. Lobar pneumonia is often due to Streptococcus pneumoniae (though Klebsiella pneumoniae is also possible.)
Multilobar pneumonia involves more than one lobe, and it often causes a more severe illness.
Bronchial pneumonia affects the lungs in patches around the tubes (bronchi or bronchioles).
Interstitial pneumonia involves the areas in between the alveoli, and it may be called "interstitial pneumonitis." It is more likely to be caused by viruses or by atypical bacteria.
The discovery of x-rays made it possible to determine the anatomic type of pneumonia without direct examination of the lungs at autopsy and led to the development of a radiological classification. Early investigators distinguished between typical lobar pneumonia and atypical (e.g. Chlamydophila) or viral pneumonia using the location, distribution, and appearance of the opacities they saw on chest x-rays. Certain x-ray findings can be used to help predict the course of illness, although it is not possible to clearly determine the microbiologic cause of a pneumonia with x-rays alone.
With the advent of modern microbiology, classification based upon the causative microorganism became possible. Determining which microorganism is causing an individual's pneumonia is an important step in deciding treatment type and length. Sputum cultures, blood cultures, tests on respiratory secretions, and specific blood tests are used to determine the microbiologic classification. Because such laboratory testing typically takes several days, microbiologic classification is usually not possible at the time of initial diagnosis.
Combined clinical classification
Traditionally, clinicians have classified pneumonia by clinical characteristics, dividing them into "acute" (less than three weeks duration) and "chronic" pneumonias. This is useful because chronic pneumonias tend to be either non-infectious, or mycobacterial, fungal, or mixed bacterial infections caused by airway obstruction. Acute pneumonias are further divided into the classic bacterial bronchopneumonias (such asStreptococcus pneumoniae), the atypical pneumonias (such as the interstitial pneumonitis of Mycoplasma pneumoniae or Chlamydia pneumoniae), and the aspiration pneumonia syndromes.
Chronic pneumonias, on the other hand, mainly include those of Nocardia, Actinomyces and Blastomyces dermatitidis, as well as the granulomatous pneumonias (Mycobacterium tuberculosis and atypical mycobacteria, Histoplasma capsulatum and Coccidioides immitis).
The combined clinical classification, now the most commonly used classification scheme, attempts to identify a person's risk factors when he or she first comes to medical attention. The advantage of this classification scheme over previous systems is that it can help guide the selection of appropriate initial treatments even before the microbiologic cause of the pneumonia is known. There are two broad categories of pneumonia in this scheme: community-acquired pneumonia and hospital-acquired pneumonia. A recently introduced type of healthcare-associated pneumonia (in patients living outside the hospital who have recently been in close contact with the health care system) lies between these two categories.
Community-acquired pneumonia
Community-acquired pneumonia (CAP) is infectious pneumonia in a person who has not recently been hospitalized. CAP is the most common type of pneumonia. The most common causes of CAP vary depending on a person's age, but they include Streptococcus pneumoniae, viruses, the atypical bacteria, and Haemophilus influenzae. Overall, Streptococcus pneumoniae is the most common cause of community-acquired pneumonia worldwide. Gram-negative bacteria cause CAP in certain at-risk populations. CAP is the fourth most common cause of death in the United Kingdom and the sixth in the United States. The term "walking pneumonia" has been used to describe a type of community-acquired pneumonia of less severity (because of the fact that the sufferer can continue to "walk" rather than require hospitalization). Walking pneumonia is usually caused by the atypical bacteria mycoplasma pneumonia.
Hospital-acquired pneumonia
Hospital-acquired pneumonia, also called nosocomial pneumonia, is pneumonia acquired during or after hospitalization for another illness or procedure with onset at least 72 hrs after admission. The causes, microbiology, treatment and prognosis are different from those of community-acquired pneumonia. Up to 5% of patients admitted to a hospital for other causes subsequently develop pneumonia. Hospitalized patients may have many risk factors for pneumonia, including mechanical ventilation, prolonged malnutrition, underlying heart and lung diseases, decreased amounts of stomach acid, and immune disturbances. Additionally, the microorganisms a person is exposed to in a hospital are often different from those at home . Hospital-acquired microorganisms may include resistant bacteria such as MRSA, Pseudomonas, Enterobacter, andSerratia. Because individuals with hospital-acquired pneumonia usually have underlying illnesses and are exposed to more dangerous bacteria, it tends to be more deadly than community-acquired pneumonia.Ventilator-associated pneumonia (VAP) is a subset of hospital-acquired pneumonia. VAP is pneumonia which occurs after at least 48 hours of intubation and mechanical ventilation.
Other types of pneumonia
Severe acute respiratory syndrome (SARS)
SARS is a highly contagious and deadly type of pneumonia which first occurred in 2002 after initial outbreaks in China. SARS is caused by the SARS coronavirus, a previously unknown pathogen.
Bronchiolitis obliterans organizing pneumonia (BOOP)
BOOP is caused by inflammation of the small airways of the lungs. It is also known as cryptogenic organizing pneumonitis (COP).
Eosinophilic pneumonia
Eosinophilic pneumonia is invasion of the lung by eosinophils, a particular kind of white blood cell. Eosinophilic pneumonia often occurs in response to infection with a parasite or after exposure to certain types of environmental factors.
Chemical pneumonia
Chemical pneumonia (usually called chemical pneumonitis) is caused by chemical toxicants such as pesticides, which may enter the body by inhalation or by skin contact. When the toxic substance is an oil, the pneumonia may be called lipoid pneumonia.
Aspiration pneumonia
Aspiration pneumonia (or aspiration pneumonitis) is caused by aspirating foreign objects which are usually oral or gastric contents, either while eating, or after reflux or vomiting which results inbronchopneumonia. The resulting lung inflammation is not an infection but can contribute to one, since the material aspirated may contain anaerobic bacteria or other unusual causes of pneumonia. Aspiration is a leading cause of death among hospital and nursing home patients, since they often cannot adequately protect their airways and may have otherwise impaired defenses.
Dust pneumonia
Dust pneumonia describes disorders caused by excessive exposure to dust storms, particularly during the Dust Bowl in the United States. With dust pneumonia, dust settles all the way into the alveoli of the lungs, stopping the cilia from moving and preventing the lungs from ever clearing themselves.
Necrotizing pneumonia, although overlapping with many other classifications, includes pneumonias that cause substantial necrosis of lung cells, and sometimes even lung abscess. Implicated bacteria are extremely commonly anaerobic bacteria, with or without additional facultatively anaerobic ones like Staphylococcus aureus, Klebsiella pneumoniae and Streptococcus pyogenes. Type 3 pneumococcus is uncommonly implicated.
Opportunistic pneumonia includes those that frequently strike immunocompromised victims. Main pathogens are cytomegalovirus, Pneumocystis jiroveci, Mycobacterium avium-intracellulare, invasiveaspergillosis, invasive candidiasis, as well as the "usual bacteria" that strike immunocompetent people as well.
USMLE case: surgery or medicine
Reply post comment
Seasonal hyperacute panuveitis (SHAPU) In Nepal

Seasonal hyperacute panuveitis (SHAPU), characterized by an unusual form of unilateral severe hyper acute diffused intraocular inflammation, is one of the mysterious eye diseases of which the definite cause and treatment remains yet to be tound out. In this study, a total of six cases were included. Aqueous and vitreous samples were subjected to direct microscopy and culture (bacterial or fungal). Of the six cases included, two yielded Streptococcus pneumoniae and one Acinetobactor sp. on culture. All three culture positive samples showed pus cells in direct microscopic examination (gram stain). All cases were subjected to vitrectomy and intravitreal antibiotic and steroid injection, along with oral antibiotics and steroid. Five cases were also treated with antiviral agent. After treatment four cases showed reversal of hypotony and three cases recovered some vision.
Moths have been reported to increase the prevalence of this disease. Complications can be as devastating as blindness.
Read NMJ journal Article...Read
Swine Flu 4 vaccines Declared
The US Food and Drug Administration (FDA) announced today that it has approved 4 vaccines against the 2009 influenza A (H1N1) virus, formerly known as "swine flu." The vaccine lots are expected to be available and distributed within the next 4 weeks.
FDA Commissioner of Food and Drugs Margaret A. Hamburg, MD, said she thought Tuesday's approval was good news for the nation's response to the H1N1 influenza virus. "This vaccine will help protect individuals from serious illness and death from influenza," she said.
The approval comes at a time when the Centers for Disease Control and Prevention (CDC) is reporting that visits to physicians around the country for influenza-like illness are increasing and are higher than expected at this time of year. The vaccines that are currently available against 3 seasonal influenza virus strains will not protect against the 2009 H1N1 virus.
The FDA said that the vaccines, based on early data, effectively elicit an immune response in most healthy adults about 8 to10 days after vaccination. Clinical studies are still underway to produce an optimal dose for children, with results expected in the near future.
Meanwhile, the CDC stresses that influenza is primarily spread through person-to-person contact, by the coughing or sneezing of infected people, and recommends that infected people stay home and limit their contact with others to keep from infecting them.
The newly approved vaccines are being made by CSL Limited, MedImmune LLC, Novartis Vaccines and Diagnostics Limited, and Sanofi Pasteur Inc. All 4 firms reportedly use the same processes to manufacture the H1N1 vaccines. As with the seasonal influenza vaccine, some lots of the H1N1 vaccine will contain the preservative thimerosal and others will not. The FDA has been continuing its efforts toward reducing thimerosal used in vaccines.
The FDA warns that persons with known allergies to chicken eggs or any other substance in the vaccine should probably not be vaccinated, although in the ongoing clinical trials, the vaccines have been well tolerated. The most common adverse effect is soreness at the injection site; other adverse effects can include a mild fever, body aches, and fatigue for a couple of days after vaccination. For the nasal spray delivery system, the most common adverse effects were runny nose, nasal congestion in all ages, sore throats in adults, and fever in children aged 2 to 6 years.
The FDA is working with different organizations regarding adverse event monitoring, information sharing, and an overall analysis during and after the 2009 H1N1 vaccination program, according to the news release. "As with any medical product, unexpected or rare serious adverse events may occur," the FDA notes.
Tonsillectomy surgery Best Video
3 minutes video, Details video
Tetralogy of Fallot


is the most common Cyanotic heart disease in children. The condition causes mixing of deoxygenated blood with the oxygenated blood being pumped out of the heart and into the circulatory system of blood vessels, Causing-
- hypoxemia.
- cyanosis, a bluish color of the skin, lips, and membranes inside the mouth and nose.
- Right ventricular hypertrophy: Narrowing or blockage of the pulmonary valve and/or muscle under the pulmonary valve coming out of the right ventricle. This restriction to blood outflow causes an increase in right ventricular work and pressure, leading to right ventricular thickening or hypertrophy.
- Ventricular septal defect (VSD): This is a hole in the heart wall (septum) that separates the 2 ventricles. The hole is usually large and allows oxygen-poor blood in the right ventricle to pass through, mixing with oxygen-rich blood in the left ventricle. This poorly oxygenated blood is then pumped out of the left ventricle to the rest of the body. The body gets some oxygen, but not all that it needs. This lack of oxygen in the blood causes cyanosis.
- Abnormal position of the aorta: The aorta, the main artery carrying blood out of the heart and into the circulatory system, exits the heart from a position overriding the right and left ventricles. (In the normal heart, the aorta exits from the left ventricle.) This is not of major importance in infants.
- Pulmonary valve stenosis (PS): The major issue with tetralogy of Fallot is the degree of pulmonary valve stenosis, since VSD is always present. If the stenosis is mild, minimal cyanosis occurs, since blood still mostly travels to the lungs. However, if the PS is moderate to severe, a smaller amount of blood reaches the lungs, since most is shunted right-to-left through the VSD
CXR - baseline
ECG - yearly to assess rhythm and QRS duration
TTE - regularly (yearly or more frequent if severe PR and RV dysfunction, can be 2 or 3 yearly if very good surgical result and no new symptoms) (NB. It is easy to under estimate the degree of PR by colour follow alone) To assess pulmonary valve function, proximal PA anatomy, RV size and function, LV function, aortic root size and degree of aortic regurgitation.
Catheterisation - for dilatation / stenting of pulmonary arteries
MRI - becoming investigation of choice for proximal pulmonary artery anatomy, RV size and function and assessment of pulmonary regurgitation
Holter - for symptoms and screening for VT or high grade ectopy in those with marked RV dilatation or QRS > 180ms
Exercise test / CPEX - exercise capacity serial assessment, pre-pregnancy counselling
Additional investigations - EP studies for those with symptomatic atrial or ventricular arrhythmias or unexplained syncope or pre-syncope
Indications for intervention
Unrepaired tetralogy of Fallot (at any age)
Significant RVOT or branch PA stenosis (RV pressure > half systemic)
Severe pulmonary regurgitation with dilatation and dysfunction of the RV
Aortic regurgitation
Arrhythmias in presence of repairable haemodynamic sequela
TREATMENT OPTIONS
Surgery (+/- anti-arrhythmia procedures)
Percutaneous pulmonary valve implantation (for those with an RV to PA conduit of suitable size only)
Percutaneous pulmonary artery angioplasty and stenting
Rickets: Clinical features Photo Gallery
Paediatric Case: Your Diagnosis 1

Diagnosis?
Rickets: Clinical Features

- Head
- Skull - Craniotabes may occur, in which the bones of the skull soften and flattening of the posterior skull can be seen. These effects may be transient or permanent. Another feature is the prominence of the frontal bones and the major foramen, resulting in frontal bossing or a prominent, sometimes square, forehead (caput quadratum).
- Teeth - Teeth may erupt later than normal because of undermineralization. Enamel can be of poor quality, resulting in caries.
- Thorax
- Rachitic rosary - The enlarged ends of the ribs, resembling beads, can be palpable and visible at the costochondral junction. As a result, the sternum can become more prominent, leading to a pigeon breast or pectus carinatum appearance.
- Harrison groove - The groove is a semicoronal impression over the abdomen at the level of the insertion of the diaphragm, which can be seen in rickets.
- Spine - A mild to more pronounced scoliosis may be seen as a result of rickets.
- Pelvis - A prominent promontory can be found, and the anteroposterior (AP) diameter of the pelvis can shrink as a result of scoliosis. If this persists in girls, it can cause complications later in life during childbirth.
- Extremities
- Arms
- Bowing of the long bones, as a reaction to greenstick fractures, results from concurrent osteomalacia.
- Thickening of the wrist at the level of the epiphysis is not visible radiographically, since the lesion consists of cartilage, although fraying and cupping of the metaphysis is evident.
- Legs
- Bowing of the long bones (genu varum)as a result of weight bearing is typical.
- Anterior bowing of the tibia (saber shin deformity) may occur.
- Development of knock-knees (genu valgum) may occur because of displacement of the growth plates during active disease.
- Thickening at the level of the ankle may occur, identical to the process in the wrist.
- Arms
- Ligaments and muscles - Laxity in the ligaments is increased, and muscle tone is decreased. This combination leads to a delay in motor development.
11 Categories Of Rickets
Because rickets results from a metabolic disturbance, the underlying disease should be diagnosed. The causes of rickets can be classified into 11 main categories:
- Vitamin D deficiency
- Dietary deficiency
- Deficient endogenous synthesis
- Gastrointestinal tract disorders
- Small intestine diseases with malabsorption
- Partial or total gastrectomy
- Hepatobiliary disease
- Chronic pancreatic insufficiency
- Disorders of vitamin D metabolism
- Hereditary - Pseudovitamin D deficiency or vitamin D dependency (types I and II)
- Acquired
- Use of anticonvulsants
- Chronic renal failure
- Acidosis
- Distal renal tubular acidosis (classic or type I)
- Secondary forms of renal acidosis
- Ureterosigmoidostomy
- Drug-induced disease
- Chronic acetazolamine ingestion
- Chronic ammonium chloride ingestion
- Chronic renal failure
- Phosphate depletion
- Dietary - Low phosphate intake plus ingestion of nonabsorbable antacids
- Hereditary - X-linked hypophosphatemic rickets or adult-onset vitamin D–resistant hypophosphatemic osteomalacia
- Acquired - Sporadic hypophosphatemic osteomalacia (phosphate diabetes), tumor-associated (oncogenous) rickets, osteomalacia, neurofibromatosis, and fibrous dysplasia
- Dietary - Low phosphate intake plus ingestion of nonabsorbable antacids
- Generalized renal tube disorders
- Primary renal tube disorders
- Renal tube disorders associated with systemic metabolic abnormality
- Cystinosis
- Glycogenosis
- Lowe syndrome
- Systemic disorder with associated renal disease
- Hereditary - Inborn errors (Wilson disease, tyrosinemia) and neurofibromatosis
- Acquired - Multiple myeloma, nephrotic syndrome, and kidney transplantation
- Intoxication-related - Cadmium, lead, outdated tetracycline
- Primary mineralization defects
- Hereditary
- Acquired
- Diphosphonate treatment
- Fluoride treatment
- States of rapid bone formation with or without a relative defect in bone resorption
- Postoperative hyperparathyroidism with osteitis fibrosa cystica
- Osteopetrosis
- Defective matrix synthesis - Fibrogenesis imperfecta ossium
- Miscellaneous
- Magnesium-dependent conditions
- Axial osteomalacia
- Parenteral alimentation
- Aluminum intoxication
- Isofosfamide treatment
Fat Soluble Vitamins: ADEK and deficiency Symptoms
Acne, allergies, loss of appetite, blindness, colds, dry hair, eye sties, fatigue, insomnia, impaired growth, itching and burning eyes, loss of smell, night blindness, dry skin, sinus trouble, steroid synthesis reduction; Decreased immune system function, cancer susceptibility. (Vitamin A is essential for bones and teeth and protects against cold and flu.)
Vitamin D deficiency
DEFICIENCY SYMPTOMS:Brittle and fragile bones, burning in mouth and throat, diarrhea, insomnia, irregular heartbeat, low blood calcium, myopia, nervousness, pale skin, poor metabolism, rickets, sensitivity to pain, soft bones and teeth, Osteoporosis and Osteopenia, and hypocalcemia. Vitamin D also enhances the immune system
Vitamin E Deficiency:
DEFICIENCY SYMPTOMS:Enlarged prostate gland, gastrointestinal disease, dry or falling out hair, impotency, miscarriages, muscular wasting, muscle weakness, sterility. Decreased circulation, slow tissue healing, leg cramps. Vitamin E helps prevent cancer, cardiovascular disease, cataracts and reduces scarring from some wounds. Zinc and Vitamin E work together.
Vitamin K deficiency:
DEFICIENCY SYMPTOMS:Brittle or fragile bones, low platelet count in blood and poor blood clotting, high glucose in blood. Vitamin K plays an essential role in blood clotting and bone formation. Can help to prevent osteoporosis. Vitamin K also converts glucose into glycogen for storage in the liver.
Magic Johnson: Fight Against HIV/AIDS

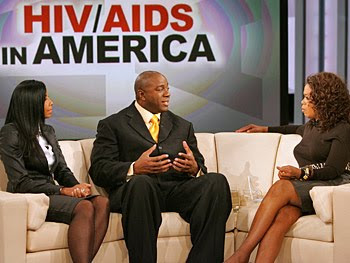
Magic Johnson: Personal life and His Commitment against AIDS
Personal life
Johnson first fathered a son in 1981, when Andre Johnson was born to Melissa Mitchell. Although Andre was raised by his mother, he visited Johnson each summer, and as of October 2005 was working for Magic Johnson Enterprises as a marketing director. In 1991, Johnson married Earlitha "Cookie" Kelly, with whom he had one son, Earvin III; the couple adopted a daughter, Elisa, in 1995.
In 1998, Johnson hosted a late night talk show on the Fox network called The Magic Hour, but the show was canceled after two months due to low ratings. He runs Magic Johnson Enterprises, a company that has a net worth of $700 million; its subsidiaries include Magic Johnson Productions, a promotional company; Magic Johnson Theaters, a nationwide chain of movie theaters; and Magic Johnson Entertainment, a movie studio. Johnson has also worked as a motivational speaker. He is a supporter of the Democratic Party—in 2005, he publicly endorsed Phil Angelides for governor of California, and Hillary Clinton for president of the United States. Johnson was an NBA commentator for Turner Network Television for seven years, before becoming a studio analyst for ESPN's NBA Countdown in 2008.
After announcing his infection in November 1991, Johnson created the Magic Johnson Foundation to help combat HIV, although he later diversified the foundation to include other charitable goals. In 1992, he joined the National Commission on AIDS, but left after eight months, saying that the commission was not doing enough to combat the disease. He was also the main speaker for the United Nations (UN) World AIDS Day Conference in 1999, and has served as a United Nations Messenger of Peace.
HIV had been associated with drug addicts and homosexuals, but Johnson's campaigns sought to show that the risk of infection was not limited to those groups. Johnson stated that his aim was to "help educate all people about what [HIV] is about" and teach others not to "discriminate against people who have HIV and AIDS". Johnson was later criticized by the AIDS community for his decreased involvement in publicizing the spread of the disease.
To prevent his HIV infection from becoming AIDS, Johnson takes a daily combination of drugs from GlaxoSmithKline and Abbott Laboratories. He has advertised GlaxoSmithKline's drugs,[91] and partnered with Abbott Laboratories to publicize the fight against AIDS in African American communities.
Schizophrenia : Diagnostic Criteria

According to the revised fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR), to be diagnosed with schizophrenia, three diagnostic criteria must be met:
- Characteristic symptoms: Two or more of the following, each present for much of the time during a one-month period (or less, if symptoms remitted with treatment).
- Delusions
- Hallucinations
- Disorganized speech, which is a manifestation of formal thought disorder
- Grossly disorganized behavior (e.g. dressing inappropriately, crying frequently) or catatonic behavior
- Negative symptoms—affective flattening (lack or decline in emotional response), alogia (lack or decline in speech), or avolition (lack or decline in motivation)
- If the delusions are judged to be bizarre, or hallucinations consist of hearing one voice participating in a running commentary of the patient's actions or of hearing two or more voices conversing with each other, only that symptom is required above. The speech disorganization criterion is only met if it is severe enough to substantially impair communication.
- Social/occupational dysfunction: For a significant portion of the time since the onset of the disturbance, one or more major areas of functioning such as work, interpersonal relations, or self-care, are markedly below the level achieved prior to the onset.
- Duration: Continuous signs of the disturbance persist for at least six months. This six-month period must include at least one month of symptoms (or less, if symptoms remitted with treatment).
Depression : You know when you have it
Symptoms of depression include:
Main Symptoms
- Mood:Feeling sad or down
- Interest:Loss of interest in normal daily activities
- Sleep: Excessive sleeping or loss of sleep.
- Concentration: poor or decreases
- Appetite: decrease appetite, smtimes overeating
- Guilt: Feeling of worthlessness
- Energy: Decrease level of energy
- Suicidal tendency
Insight is always present except in manic depression
Questions to ask your self.
| How much of the time... | All of the time | Most of the time | More than half of the time | Less than half of the time | Some of the time | At no time | |
| 1 | Have you felt in low spirits or sad? | 5 | 4 | 3 | 2 | 1 | 0 |
| 2 | Have you lost interest in your daily activities? | 5 | 4 | 3 | 2 | 1 | 0 |
| 3 | Have you felt lacking in energy and strength? | 5 | 4 | 3 | 2 | 1 | 0 |
| 4 | Have you felt less self-confident? | 5 | 4 | 3 | 2 | 1 | 0 |
| 5 | Have you had a bad conscience or feelings of guilt? | 5 | 4 | 3 | 2 | 1 | 0 |
| 6 | Have you felt that life wasn't worth living? | 5 | 4 | 3 | 2 | 1 | 0 |
| 7 | Have you had difficulty in concentrating, e.g. when reading the newspaper or watching television? | 5 | 4 | 3 | 2 | 1 | 0 |
| 8a | Have you felt very restless? | 5 | 4 | 3 | 2 | 1 | 0 |
| 8b | Have you felt subdued? | 5 | 4 | 3 | 2 | 1 | 0 |
| 9 | Have you had trouble sleeping at night? | 5 | 4 | 3 | 2 | 1 | 0 |
| 10a | Have you suffered from reduced appetite? | 5 | 4 | 3 | 2 | 1 | 0 |
| 10b | Have you suffered from increased appetite? | 5 | 4 | 3 | 2 | 1 | 0 |
Others
- Feeling hopeless
- Difficulty making decisions
- Unintentional weight gain or loss
- Irritability
- Restlessness
- Being easily annoyed
- Feeling fatigued or weak
- Loss of interest in sex
- Unexplained physical problems, such as back pain or headaches
Medical Case Report 5 : with answer

CASE REPORT
A 28-year-old man with no significant previous medical history came to the emergency department with a complaint of mild sore throat that had persisted for three days, accompanied by arthralgia, myalgia, and low-grade fever. The day before, he had had a severe headache with neck stiffness, nausea, and vomiting. he claimed not to have a cough, shortness of breath, abdominal pain, diarrhea, or urinary tract symptoms. he had no history of tick exposure or skin rash, was not taking any medications, had no known drug allergies, and did not smoke. he lived with his wife and two children, all of whom were well.
On physical examination, he was thin, alert, and oriented but had an inappropriate affect. His temperature was 98.6°F; pulse, 100; respirations, 20; and blood pressure, 110/70 mm Hg. His neck was stiff, but Kernig and Brudzinski signs were not present. The pharynx was slightly injected but without exudate. Findings on heart and lung examination were normal. No rash was present. The neurologic examination revealed intact cranial nerves, normal reflexes, and no sensory or motor deficits. His white blood cell count was 21,800/mm3 with 67% polymorphonuclear leukocytes and 26% band cells. Platelet count was 200,000/mm3. Electrolyte levels were within normal range, and the glucose level was 131 mg/dL. A chest film showed no signs of pneumonia. A lumbar puncture revealed clear cerebrospinal fluid (CSF) with a glucose level of 88 mg/dL and a total protein level of 33 mg/dL and no cells.
The patient underwent intravenous hydration after he was admitted with a diagnosis of meningismus, accompanied by the instruction to "rule out early viral meningitis versus viral syndrome." Approximately 12 hours later, he became acutely lethargic and a second spinal tap was performed. The CSF appeared cloudy and now contained 871 white blood cells, of which 93% were polymorphonuclear leukocytes; the glucose level was 1 mg/dL; the total protein level, 417 mg/dL. Gram stain revealed rare gram-negative diplococci, the latex agglutination test for bacterial antigens was positive for Neisseria meningitidis, and both the original and repeated CSF cultures grew N. meningitidis.
Mx
The patient was given high-dose intravenous penicillin G, 24 million units a day, and was transferred to the medical intensive care unit for observation. Despite the 12-hour delay in diagnosis, he recovered completely. Intimate household contacts received prophylactic rifampin, and the patient was given rifampin before discharge to eliminate nasopharyngeal carriage of Neisseria.
Causes of Hemoptysis : Coughing out Blood
- Infections. These include pneumonia; tuberculosis; aspergillosis; and parasitic diseases, including ascariasis, amebiasis, and paragonimiasis.
- Tumors that erode blood vessel walls.
- Drug abuse. Cocaine can cause massive hemoptysis.
- Trauma. Chest injuries can cause bleeding into the lungs.
- Vascular disorders, including aneurysms, pulmonary embolism, and malformations of the blood vessels.
- Bronchitis. Its most common cause is long-term smoking.
- Foreign object(s) in the airway.
- Blood clotting disorders.
- Bleeding following such surgical procedures as bronchial biopsies and heart catheterization.
WHO Issues Guidelines for Antiviral Treatment for H1N1 and Other Influenza
August 25, 2009 —
The World Health Organization (WHO) has issued guidelines for antiviral treatment for novel influenza A (H1N1) and other influenza. The purpose of the new recommendations, which were posted online August 20, is to provide a basis for advice to clinicians regarding the use of the currently available antivirals for patients presenting with illness caused by influenza virus infection, as well as considerations regarding potential use of these antiviral medications for chemoprophylaxis.
On the basis of a review of data collected with previously circulating strains, and treatment of human H5N1 influenza virus infections, the new guidelines expand on recommendations published in May 2009, titled ʺClinical management of human infection with new influenza A (H1N1) virus: Initial guidance." These new guidelines do not change recommendations in the WHO rapid advice guidelines on pharmacological management of humans infected with highly pathogenic avian influenza A (H5N1) virus.
"In April 2009, the [WHO] received reports of sustained person to person infections with [H1N1] virus in Mexico and the United States," write Edgar Bautista, from Médico Neumólogo Intensivista, Jefe de UCI-INER in Mexico, and colleagues. "Subsequent international spread led WHO to declare on 11 June 2009 that the first influenza pandemic in 41 years had occurred. This 2009 pandemic H1N1 influenza virus has now spread worldwide, with confirmed cases of pandemic H1N1 virus infection reported in more than 100 countries in all 6 WHO regions[, which] has led to the need to add to the existing guidance on the use of antivirals."
The new recommendations highlight oseltamivir and zanamivir, which are neuraminidase inhibitors, and amantadine and rimantadine, which are M2 inhibitors. Suggestions are also provided regarding the use of some other potential pharmacological treatments, such as ribavirin, interferons, immunoglobulins, and corticosteroids.
Management of patients with pandemic influenza (H1N1) 2009 virus infection is the primary focus of the statement, although it also includes guidance regarding the use of the antivirals for treatment of other seasonal influenza virus strains, as well as for infections resulting from novel influenza A virus strains.
The guidelines urge country and local public health authorities to issue local recommendations for clinicians periodically, based on epidemiological and antiviral susceptibility data on the locally circulating influenza strains. As the prevalence and severity of the current pandemic evolves, WHO anticipates that additional data will be forthcoming that may require revision of the current recommendations. WHO therefore plans to review the guidance no later than September 2009 to determine whether modifications to the recommendations are needed.
Recommendations for Antiviral Treatment of H1N1
For patients with confirmed or strongly suspected infection with influenza pandemic (H1N1) 2009, when antiviral medications for influenza are available, specific recommendations regarding use of antivirals for treatment of pandemic (H1N1) 2009 influenza virus infection are as follows:
•Oseltamivir should be prescribed, and treatment started as soon as possible, for patients with severe or progressive clinical illness (strong recommendation, low-quality evidence). Depending on clinical response, higher doses of up to 150 mg twice daily and longer duration of treatment may be indicated. This recommendation is intended for all patient groups, including pregnant women, neonates, and children younger than 5 years of age.
•Zanamivir is indicated for patients with severe or progressive clinical illness when oseltamivir is not available or not possible to use, or when the virus is resistant to oseltamivir but known or likely to be susceptible to zanamivir (strong recommendation, very low quality evidence).
•Antiviral treatment is not required in patients not in at-risk groups who have uncomplicated illness caused by confirmed or strongly suspected influenza virus infection (weak recommendation, low-quality evidence). Patients considered to be at risk are infants and children younger than 5 years of age; adults older than 65 years of age; nursing home residents; pregnant women; patients with chronic comorbid disease including cardiovascular, respiratory, or liver disease and diabetes; and immunosuppressed patients because of malignancy, HIV infection, or other diseases.
•Oseltamivir or zanamivir treatment should be started as soon as possible after the onset of illness in patients in at-risk groups who have uncomplicated illness caused by influenza virus infection (strong recommendation, very low quality evidence).
Recommendations for Chemoprophylaxis of H1N1
Specific recommendations regarding the use of antivirals for chemoprophylaxis of pandemic (H1N1) 2009 influenza virus infection are as follows:
•When risk for human-to-human transmission of influenza is high or low, and the probability of complications of infection is high, either because of the influenza strain or because of the baseline risk of the exposed group, use of oseltamivir or zanamivir may be considered as postexposure chemoprophylaxis for the affected community or group, for individuals in at-risk groups, or for healthcare workers (weak recommendation, moderate-quality evidence).
•Individuals in at-risk groups or healthcare personnel need not be offered antiviral chemoprophylaxis if the likelihood of complications of infection is low. This recommendation should be applied independent of risk for human-to-human transmission (weak recommendation, low-quality evidence).
For treatment of mild to moderate uncomplicated clinical presentation of infection with multiple cocirculating influenza A subtypes or viruses with different antiviral susceptibilities, patients in at-risk groups should be treated with zanamivir or oseltamivir plus M2 inhibitor (noting that amantadine should not be used in pregnant women). Otherwise-healthy patients with this presentation need not be treated.
When the clinical presentation of infection with multiple cocirculating influenza A subtypes or viruses with different antiviral susceptibilities is severe or progressive, all patients should be treated with oseltamivir plus M2 inhibitor, or zanamivir.
For treatment of mild to moderate uncomplicated clinical presentation of infection with sporadic zoonotic influenza A viruses including H5N1, the at-risk population should be treated with oseltamivir or zanamivir, and the otherwise-healthy population with oseltamivir. All patients, regardless of risk status, with severe or progressive presentation of infection with sporadic zoonotic influenza A viruses including H5N1 should be treated with oseltamivir plus an M2 inhibitor.
((News From MEDSCAPE NEWS))
Irrirtable Bowel Syndrome IBS : Short review and Rome II Criteria

Differential Diagnosis
Symptoms
The primary symptoms of IBS are abdominal pain or discomfort in association with frequent diarrhea or constipation, a change in bowel habits. There may also be urgency for bowel movements, a feeling of incomplete evacuation (tenesmus), bloating or abdominal distention. People with IBS more commonly than others have gastroesophageal reflux, symptoms relating to the genitourinary system, psychological symptoms, fibromyalgia, chronic fatigue syndrome, headache and backache.
Rome Process for Diagnosing IBS
The cardinal requirement for the diagnosis of IBS is abdominal pain. The Rome II criteria is used to diagnose IBS after a careful examination of the patient's medical history and physical abdominal examination which looks for any 'red flag' symptoms. More recently, the Rome III criteria, incorporating some changes over the previous set of criteria, have been issued. The Rome II and III efforts have integrated pediatric contents to their set of criteria.
According to the Rome II committees and the Functional Brain Gut Research Group, IBS can be diagnosed based on at least 12 weeks, which need not be consecutive, of the preceding 12 months there was abdominal discomfort or pain that had two out of three of these features:
Relieved with defecation; and/or
Onset associated with a change in frequency of stool; and/or
Onset associated with a change in form (appearance) of stool.
Symptoms that cumulatively support the diagnosis of IBS:
Abnormal stool frequency (for research purposes, "abnormal" may be defined as greater than 3 bowel movements per day and less than 3 bowel movements per week);
Abnormal stool form (lumpy/hard or loose/watery stool);
Abnormal stool passage (straining, urgency, or feeling of incomplete evacuation);
Bloating or feeling of abdominal distention.
Supportive symptoms of IBS:
A) Fewer than three bowel movements a week
B) More than three bowel movements a day
C) Hard or lumpy stools
D) Loose (mushy) or watery stools
E) Straining during a bowel movement
F) Urgency (having to rush to have a bowel movement)
G) Feeling of incomplete bowel movement
H) Passing mucus (white material) during a bowel movement
I) Abdominal fullness, bloating, or swelling
Diarrhea-predominant: At least 1 of B, D, F and none of A, C, E; or at least 2 of B, D, F and one of A or E.
Constipation-predominant: At least 1 of A, C, E and none of B, D, F; or at least 2 of A, C, E and one of B, D, F.
Red flag symptoms which are not typical of IBS:
Pain that awakens/interferes with sleep
Diarrhea that awakens/interferes with sleep
Blood in the stool (visible or occult)
Weight loss
Fever
Abnormal physical examination




.jpg)

















