Contact dermatitis is a localized rash or irritation of the skin caused by contact with a foreign substance. Only the superficial regions of the skin are affected in contact dermatitis. Inflammation of the affected tissue is present in the epidermis (the outermost layer of skin) and the outer dermis (the layer beneath the epidermis).Unlike contact urticaria, in which a rash appears within minutes of exposure and fades a
way within minutes to hours, contact dermatitis takes days to fade away. Even then, contact dermatitis fades only if the skin no longer comes in contact with the allergen or irritant. Contact dermatitis results in large, burning, and itchy rashes, and these can take anywhere from several days to weeks to heal. Chronic contact dermatitis can develop when the removal of the offending agent no longer provides expected relief.
Causes
In North/South America, the most common causes of allerg ic contact dermatitis are plants of the Toxicodendron genus: poison ivy, poison oak, and poison sumac. Specific plant species that can induce
ic contact dermatitis are plants of the Toxicodendron genus: poison ivy, poison oak, and poison sumac. Specific plant species that can induce
such contact dermatitis include Western Poison Oak, a widespread plant in the western USA. Common causes of irritant contact dermatitis are harsh (highly alkaline) soaps, detergents, and cleaning products.
Types of contact dermatitis
There are three types of contact dermatitis: irritant contact, allergic contact, and photocontact dermatitis. Photocontact dermatitis is divided into two categories: phototoxic and photoallergic.
Chemical irritant contact dermatitis
Physical irritant contact dermatitisPlants
Allergic contact dermatitisCommon allergens implicated include the following:
- Nickel (nickel sulfate hexahydrate) - metal frequently encountered in jewelry and clasps or buttons on clothing
- Gold (gold sodium thiosulfate) - precious metal often found in jewelry
- Balsam of Peru (Myroxylon pereirae) - a fragrance used in perfumes and skin lotions, derived from tree resin (see also Tolu balsam)
- Thimerosal - a mercury compound used in local antiseptics and in vaccines
- Neomycin - a topical antibiotic common in first aid creams and ointments, cosmetics, deodorant, soap and pet food. Found by itself, or in Polysporin or Triple Antibiotic
- Fragrance mix - a group of the eight most common fragrance allergens found in foods, cosmetic products, insecticides, antiseptics, soaps, perfumes and dental products [15]
- Formaldehyde - a preservative with multiple uses, e.g., in paper products, paints, medications, household cleaners, cosmetic products and fabric finishes
- Cobalt chloride - metal found in medical products; hair dye; antiperspirant; metal-plated objects such as snaps, buttons or tools; and in cobalt blue pigment
- Bacitracin - a topical antibiotic found by itself, or as Polysporin or Triple Antibiotic
- Quaternium-15 - preservative in cosmetic products (self-tanners, shampoo, nail polish, sunscreen) and in industrial products (polishes, paints and waxes).[16]
- Colophony (Rosin) - Rosin, sap or sawdust typically from spruce or fir trees
- Topical steroid - see steroid allergy
Photocontact Dermatitis
Sometimes termed "photoaggravated"(Bourke et al. 2001)[17], and divided into two categories, phototoxic and photoallergic, PCD is the eczematous condition which is triggered by an interaction between an otherwise unharmful or less harmful substance on the skin and ultraviolet light (320-400 nm UVA) (ESCD 2006), therefore manifesting itself only in regions where the sufferer has been exposed to such rays. Without the presence of these rays, the photosensitiser is not harmful. For this reason, this form of contact dermatitis is usually associated only with areas of skin which are left uncovered by clothing. The mechanism of action varies from toxin to toxin, but is usually due to the production of a photoproduct. Toxins which are associated with PCD include the psoralens. Psoralens are in fact used therapeutically for the treatment of psoriasis, eczema and vitiligo.
Photocontact dermatitis is another condition where the distinction between forms of contact dermatitis is not clear cut. Immunological mechanisms can also play a part, causing a response similar to ACD.
Symptoms
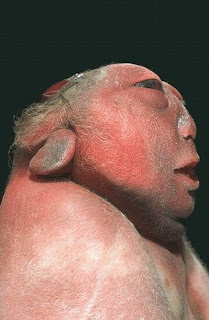
Allergic dermatitis is usually confined to the area where the trigger actually touched the skin, whereas irritant dermatitis may be more widespread on the skin. Symptoms of both forms include the following:
- Red rash. This is the usual reaction. The rash appears immediately in irritant contact dermatitis; in allergic contact dermatitis, the rash sometimes does not appear until 24–72 hours after exposure to the allergen.
- Blisters or wheals. Blisters, wheals (welts), and urticaria (hives) often form in a pattern where skin was directly exposed to the allergen or irritant.
- Itchy, burning skin. Irritant contact dermatitis tends to be more painful than itchy, while allergic contact dermatitis often itches.
While either form of contact dermatitis can affect any part of the body, irritant contact dermatitis often affects the hands, which have been exposed by resting in or dipping into a container (sink, pail, tub, Sun, Swimming Pools With High chlorine ), containing the irritant.
Treatment
Self-care at Home
- Immediately after exposure to a known allergen or irritant, wash with soap and cool water to remove or inactivate most of the offending substance.
- Weak acid solutions [lemon juice, vinegar] can be used to counteract the effects of dermatitis contracted by exposure to basic irritants [phenol etc.].
- If blistering develops, cold moist compresses applied for 30 minutes 3 times a day can offer relief.
- Calamine lotion and cool colloidal oatmeal baths may relieve itching.
- Oral antihistamines such as diphenhydramine (Benadryl, Ben-Allergin) can also relieve itching.
- For mild cases that cover a relatively small area, hydrocortisone cream in nonprescription strength may be sufficient.
- Avoid scratching, as this can cause secondary infections.
- A barrier cream such as those containing zinc oxide (e.g. Desitin, etc.) may help to protect the skin and retain moisture.
Medical Care
If the rash does not improve or continues to spread after 2-3 of days of self-care, or if the itching and/or pain is severe, the patient should contact a dermatologist or other physician or physician assistant. Medical treatment usually consists of lotions, creams, or oral medications.
- Corticosteroids. A corticosteroid medication similar to hydrocortisone may be prescribed to combat inflammation in a localized area. This medication may be applied to your skin as a cream or ointment. If the reaction covers a relatively large portion of the skin or is severe, a corticosteroid in pill or injection form may be prescribed.
- Antihistamines. Prescription antihistamines may be given if nonprescription strengths are inadequate.
Prevention
Since contact dermatitis relies on an irritant or an allergen to initiate the reaction, it is important for the patient to identify the responsible agent and avoid it. This can be accomplished by having patch tests, a method commonly known as allergy testing. The patient must know where the irritant or allergen is found to be able to avoid it. It is important to also note that chemicals sometimes have several different names.[18]
In an industrial setting the employer has a duty of care to the individual worker to provide the correct level of safety equipment to mitigate the exposure to harmful irritants. This can take the form of protective clothing, gloves or barrier cream depending on the working environment.