Guillain-Barré syndrome (GBS) is an acute inflammatory demyelinating polyneuropathy (AIDP), an autoimmune disorder affecting the peripheral nervous system, usually triggered by an acute infectious process. It is included in the wider group of peripheral neuropathies. There are several types of GBS, but unless otherwise stated, GBS refers to the most common form, AIDP. It is frequently severe and usually exhibits as an ascending paralysis noted by weakness in the legs that spreads to the upper limbs and the face along with complete loss of deep tendon reflexes. With prompt treatment by plasmapheresis or intravenous immunoglobulins and supportive care, the majority of patients will regain full functional capacity. However, death may occur if severe pulmonary complications and dysautonomia are present.
Pathophysiology
All forms of Guillain-Barré syndrome are due to an immune response to foreign antigens (such as infectious agents) that are mistargeted at host nerve tissues instead (a form of antigenic mimicry). The targets of such immune attack are thought to be gangliosides, which are complex glycosphingolipids present in large quantities on human nerve tissues, especially in the nodes of Ranvier. An example is the GM1 ganglioside, which can be affected in as many as 20-50% of cases, especially in those preceded by Campylobacter jejuni infections. Another example is the GQ1b ganglioside, which is the target in the Miller Fisher syndrome variant
The most common antecedent infection is Campylobacter jejuni. However, 60% of cases do not have a known cause.
The end result of such autoimmune attack on the peripheral nerves is inflammation of myelin and conduction block, leading to a muscle paralysis that may be accompanied by sensory or autonomic disturbances.
Serum sickness can rarely manifest as the Guillain-Barre syndrome (GBS)
Signs and symptoms - weakness which affects the lower limbs first, and rapidly progresses in an ascending fashion.
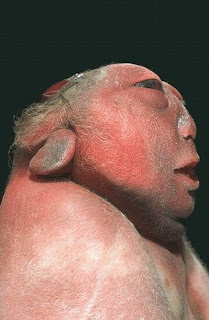
- Frequently, the lower cranial nerves may be affected, leading to bulbar weakness, (oropharyngeal dysphagia, that is difficulty with swallowing, drooling, and/or maintaining an open airway) and respiratory difficulties.
- Most patients require hospitalization and about 30% require ventilatory assistance.
- Facial weakness is also commonly a feature, but eye movement abnormalities are not commonly seen in ascending GBS, but are a prominent feature in the Miller-Fisher variant
- Sensory loss, if present, usually takes the form of loss of proprioception (position sense) and areflexia (complete loss of deep tendon reflexes), an important feature of GBS.
- Loss of pain and temperature sensation is usually mild. In fact, pain is a common symptom in GBS, presenting as deep aching pain, usually in the weakened muscles, which patients compare to the pain from overexercising.
- These pains are self-limited and should be treated with standard analgesics. Bladder dysfunction may occur in severe cases but should be transient. If severe, spinal cord disorder should be suspected.
- Fever should not be present, and if it is, another cause should be suspected.
- In severe cases of GBS, loss of autonomic function is common, manifesting as wide fluctuations in blood pressure, orthostatic hypotension, and cardiac arrhythmias.
Six different subtypes of Guillain-Barre syndrome (GBS) exist:
- Acute inflammatory demyelinating polyneuropathy (AIDP)
- Miller Fisher syndrome (MFS)
- Acute motor axonal neuropathy (AMAN)
- Acute motor sensory axonal neuropathy (AMSAN)
- Acute panautonomic neuropathy
- Bickerstaff’s brainstem encephalitis (BBE)
Diagnosis
The diagnosis of GBS usually depends on findings such as rapid development of muscle paralysis, areflexia, absence of fever, and a likely inciting event. CSF and ECD is used almost every time to verify symptoms, but because of the acute nature of the disorder, they may not become abnormal until after the first week of onset of signs and symptoms.
There currently is no cure for Guillain-Barre syndrome. However, treatments have been proven effective against this syndrome.
- Typical CSF findings include albumino-cytological dissociation. As opposed to infectious causes, this is an elevated protein level (100 - 1000 mg/dL), without an accompanying pleocytosis (increased cell count). A sustained pleocytosis may indicate an alternative diagnosis such as infection.
Electrodiagnostics
- Electromyography (EMG) and nerve conduction study (NCS) may show prolonged distal latencies, conduction slowing, conduction block, and temporal dispersion of compound action potential in demyelinating cases. In primary axonal damage, the findings include reduced amplitude of the action potentials without conduction slowing.
Diagnostic criteria
Required
- Progressive, relatively symmetrical weakness of 2 or more limbs due to neuropathy
- Areflexia
- Disorder course <>
- Exclusion of other causes (see below)
Supportive
- relatively symmetric weakness accompanied by numbness and/or tingling
- mild sensory involvement
- facial nerve or other cranial nerve involvement
- absence of fever
- typical CSF findings obtained from lumbar puncture
- electrophysiologic evidence of demyelination from electromyogram
Treatment Supportive care with monitoring of all vital functions is the cornerstone of successful management in the acute patient. Of greatest concern is respiratory failure due to paralysis of the diaphragm.
Early intubation should be considered in any patient with a vital capacity (VC) <20>2O, more than 30% decrease in either VC or NIF within 24 hours, rapid progression of disorder, or autonomic instability.
Once the patient is stabilized, treatment of the underlying condition should be initiated as soon as possible.
Either high-dose intravenous immunoglobulins (IVIg) at 400 mg/kg for 5 days or
plasmapheresis