
Medicine, surgery,ophthalmology,psychiatry,dermatology,ENT disease,treatment,cure,diagnosis,complications, Medical cases Ebooks free downloads medical videos Gallery
Magic Johnson: Fight Against HIV/AIDS

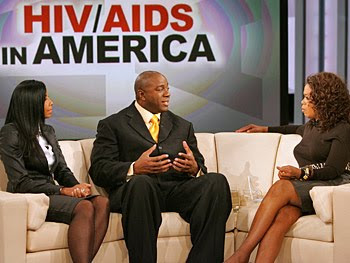
Magic Johnson: Personal life and His Commitment against AIDS
Personal life
Johnson first fathered a son in 1981, when Andre Johnson was born to Melissa Mitchell. Although Andre was raised by his mother, he visited Johnson each summer, and as of October 2005 was working for Magic Johnson Enterprises as a marketing director. In 1991, Johnson married Earlitha "Cookie" Kelly, with whom he had one son, Earvin III; the couple adopted a daughter, Elisa, in 1995.
In 1998, Johnson hosted a late night talk show on the Fox network called The Magic Hour, but the show was canceled after two months due to low ratings. He runs Magic Johnson Enterprises, a company that has a net worth of $700 million; its subsidiaries include Magic Johnson Productions, a promotional company; Magic Johnson Theaters, a nationwide chain of movie theaters; and Magic Johnson Entertainment, a movie studio. Johnson has also worked as a motivational speaker. He is a supporter of the Democratic Party—in 2005, he publicly endorsed Phil Angelides for governor of California, and Hillary Clinton for president of the United States. Johnson was an NBA commentator for Turner Network Television for seven years, before becoming a studio analyst for ESPN's NBA Countdown in 2008.
After announcing his infection in November 1991, Johnson created the Magic Johnson Foundation to help combat HIV, although he later diversified the foundation to include other charitable goals. In 1992, he joined the National Commission on AIDS, but left after eight months, saying that the commission was not doing enough to combat the disease. He was also the main speaker for the United Nations (UN) World AIDS Day Conference in 1999, and has served as a United Nations Messenger of Peace.
HIV had been associated with drug addicts and homosexuals, but Johnson's campaigns sought to show that the risk of infection was not limited to those groups. Johnson stated that his aim was to "help educate all people about what [HIV] is about" and teach others not to "discriminate against people who have HIV and AIDS". Johnson was later criticized by the AIDS community for his decreased involvement in publicizing the spread of the disease.
To prevent his HIV infection from becoming AIDS, Johnson takes a daily combination of drugs from GlaxoSmithKline and Abbott Laboratories. He has advertised GlaxoSmithKline's drugs,[91] and partnered with Abbott Laboratories to publicize the fight against AIDS in African American communities.
Schizophrenia : Diagnostic Criteria

According to the revised fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR), to be diagnosed with schizophrenia, three diagnostic criteria must be met:
- Characteristic symptoms: Two or more of the following, each present for much of the time during a one-month period (or less, if symptoms remitted with treatment).
- Delusions
- Hallucinations
- Disorganized speech, which is a manifestation of formal thought disorder
- Grossly disorganized behavior (e.g. dressing inappropriately, crying frequently) or catatonic behavior
- Negative symptoms—affective flattening (lack or decline in emotional response), alogia (lack or decline in speech), or avolition (lack or decline in motivation)
- If the delusions are judged to be bizarre, or hallucinations consist of hearing one voice participating in a running commentary of the patient's actions or of hearing two or more voices conversing with each other, only that symptom is required above. The speech disorganization criterion is only met if it is severe enough to substantially impair communication.
- Social/occupational dysfunction: For a significant portion of the time since the onset of the disturbance, one or more major areas of functioning such as work, interpersonal relations, or self-care, are markedly below the level achieved prior to the onset.
- Duration: Continuous signs of the disturbance persist for at least six months. This six-month period must include at least one month of symptoms (or less, if symptoms remitted with treatment).
Depression : You know when you have it
Symptoms of depression include:
Main Symptoms
- Mood:Feeling sad or down
- Interest:Loss of interest in normal daily activities
- Sleep: Excessive sleeping or loss of sleep.
- Concentration: poor or decreases
- Appetite: decrease appetite, smtimes overeating
- Guilt: Feeling of worthlessness
- Energy: Decrease level of energy
- Suicidal tendency
Insight is always present except in manic depression
Questions to ask your self.
| How much of the time... | All of the time | Most of the time | More than half of the time | Less than half of the time | Some of the time | At no time | |
| 1 | Have you felt in low spirits or sad? | 5 | 4 | 3 | 2 | 1 | 0 |
| 2 | Have you lost interest in your daily activities? | 5 | 4 | 3 | 2 | 1 | 0 |
| 3 | Have you felt lacking in energy and strength? | 5 | 4 | 3 | 2 | 1 | 0 |
| 4 | Have you felt less self-confident? | 5 | 4 | 3 | 2 | 1 | 0 |
| 5 | Have you had a bad conscience or feelings of guilt? | 5 | 4 | 3 | 2 | 1 | 0 |
| 6 | Have you felt that life wasn't worth living? | 5 | 4 | 3 | 2 | 1 | 0 |
| 7 | Have you had difficulty in concentrating, e.g. when reading the newspaper or watching television? | 5 | 4 | 3 | 2 | 1 | 0 |
| 8a | Have you felt very restless? | 5 | 4 | 3 | 2 | 1 | 0 |
| 8b | Have you felt subdued? | 5 | 4 | 3 | 2 | 1 | 0 |
| 9 | Have you had trouble sleeping at night? | 5 | 4 | 3 | 2 | 1 | 0 |
| 10a | Have you suffered from reduced appetite? | 5 | 4 | 3 | 2 | 1 | 0 |
| 10b | Have you suffered from increased appetite? | 5 | 4 | 3 | 2 | 1 | 0 |
Others
- Feeling hopeless
- Difficulty making decisions
- Unintentional weight gain or loss
- Irritability
- Restlessness
- Being easily annoyed
- Feeling fatigued or weak
- Loss of interest in sex
- Unexplained physical problems, such as back pain or headaches
Medical Case Report 5 : with answer

CASE REPORT
A 28-year-old man with no significant previous medical history came to the emergency department with a complaint of mild sore throat that had persisted for three days, accompanied by arthralgia, myalgia, and low-grade fever. The day before, he had had a severe headache with neck stiffness, nausea, and vomiting. he claimed not to have a cough, shortness of breath, abdominal pain, diarrhea, or urinary tract symptoms. he had no history of tick exposure or skin rash, was not taking any medications, had no known drug allergies, and did not smoke. he lived with his wife and two children, all of whom were well.
On physical examination, he was thin, alert, and oriented but had an inappropriate affect. His temperature was 98.6°F; pulse, 100; respirations, 20; and blood pressure, 110/70 mm Hg. His neck was stiff, but Kernig and Brudzinski signs were not present. The pharynx was slightly injected but without exudate. Findings on heart and lung examination were normal. No rash was present. The neurologic examination revealed intact cranial nerves, normal reflexes, and no sensory or motor deficits. His white blood cell count was 21,800/mm3 with 67% polymorphonuclear leukocytes and 26% band cells. Platelet count was 200,000/mm3. Electrolyte levels were within normal range, and the glucose level was 131 mg/dL. A chest film showed no signs of pneumonia. A lumbar puncture revealed clear cerebrospinal fluid (CSF) with a glucose level of 88 mg/dL and a total protein level of 33 mg/dL and no cells.
The patient underwent intravenous hydration after he was admitted with a diagnosis of meningismus, accompanied by the instruction to "rule out early viral meningitis versus viral syndrome." Approximately 12 hours later, he became acutely lethargic and a second spinal tap was performed. The CSF appeared cloudy and now contained 871 white blood cells, of which 93% were polymorphonuclear leukocytes; the glucose level was 1 mg/dL; the total protein level, 417 mg/dL. Gram stain revealed rare gram-negative diplococci, the latex agglutination test for bacterial antigens was positive for Neisseria meningitidis, and both the original and repeated CSF cultures grew N. meningitidis.
Mx
The patient was given high-dose intravenous penicillin G, 24 million units a day, and was transferred to the medical intensive care unit for observation. Despite the 12-hour delay in diagnosis, he recovered completely. Intimate household contacts received prophylactic rifampin, and the patient was given rifampin before discharge to eliminate nasopharyngeal carriage of Neisseria.
Causes of Hemoptysis : Coughing out Blood
- Infections. These include pneumonia; tuberculosis; aspergillosis; and parasitic diseases, including ascariasis, amebiasis, and paragonimiasis.
- Tumors that erode blood vessel walls.
- Drug abuse. Cocaine can cause massive hemoptysis.
- Trauma. Chest injuries can cause bleeding into the lungs.
- Vascular disorders, including aneurysms, pulmonary embolism, and malformations of the blood vessels.
- Bronchitis. Its most common cause is long-term smoking.
- Foreign object(s) in the airway.
- Blood clotting disorders.
- Bleeding following such surgical procedures as bronchial biopsies and heart catheterization.
WHO Issues Guidelines for Antiviral Treatment for H1N1 and Other Influenza
August 25, 2009 —
The World Health Organization (WHO) has issued guidelines for antiviral treatment for novel influenza A (H1N1) and other influenza. The purpose of the new recommendations, which were posted online August 20, is to provide a basis for advice to clinicians regarding the use of the currently available antivirals for patients presenting with illness caused by influenza virus infection, as well as considerations regarding potential use of these antiviral medications for chemoprophylaxis.
On the basis of a review of data collected with previously circulating strains, and treatment of human H5N1 influenza virus infections, the new guidelines expand on recommendations published in May 2009, titled ʺClinical management of human infection with new influenza A (H1N1) virus: Initial guidance." These new guidelines do not change recommendations in the WHO rapid advice guidelines on pharmacological management of humans infected with highly pathogenic avian influenza A (H5N1) virus.
"In April 2009, the [WHO] received reports of sustained person to person infections with [H1N1] virus in Mexico and the United States," write Edgar Bautista, from Médico Neumólogo Intensivista, Jefe de UCI-INER in Mexico, and colleagues. "Subsequent international spread led WHO to declare on 11 June 2009 that the first influenza pandemic in 41 years had occurred. This 2009 pandemic H1N1 influenza virus has now spread worldwide, with confirmed cases of pandemic H1N1 virus infection reported in more than 100 countries in all 6 WHO regions[, which] has led to the need to add to the existing guidance on the use of antivirals."
The new recommendations highlight oseltamivir and zanamivir, which are neuraminidase inhibitors, and amantadine and rimantadine, which are M2 inhibitors. Suggestions are also provided regarding the use of some other potential pharmacological treatments, such as ribavirin, interferons, immunoglobulins, and corticosteroids.
Management of patients with pandemic influenza (H1N1) 2009 virus infection is the primary focus of the statement, although it also includes guidance regarding the use of the antivirals for treatment of other seasonal influenza virus strains, as well as for infections resulting from novel influenza A virus strains.
The guidelines urge country and local public health authorities to issue local recommendations for clinicians periodically, based on epidemiological and antiviral susceptibility data on the locally circulating influenza strains. As the prevalence and severity of the current pandemic evolves, WHO anticipates that additional data will be forthcoming that may require revision of the current recommendations. WHO therefore plans to review the guidance no later than September 2009 to determine whether modifications to the recommendations are needed.
Recommendations for Antiviral Treatment of H1N1
For patients with confirmed or strongly suspected infection with influenza pandemic (H1N1) 2009, when antiviral medications for influenza are available, specific recommendations regarding use of antivirals for treatment of pandemic (H1N1) 2009 influenza virus infection are as follows:
•Oseltamivir should be prescribed, and treatment started as soon as possible, for patients with severe or progressive clinical illness (strong recommendation, low-quality evidence). Depending on clinical response, higher doses of up to 150 mg twice daily and longer duration of treatment may be indicated. This recommendation is intended for all patient groups, including pregnant women, neonates, and children younger than 5 years of age.
•Zanamivir is indicated for patients with severe or progressive clinical illness when oseltamivir is not available or not possible to use, or when the virus is resistant to oseltamivir but known or likely to be susceptible to zanamivir (strong recommendation, very low quality evidence).
•Antiviral treatment is not required in patients not in at-risk groups who have uncomplicated illness caused by confirmed or strongly suspected influenza virus infection (weak recommendation, low-quality evidence). Patients considered to be at risk are infants and children younger than 5 years of age; adults older than 65 years of age; nursing home residents; pregnant women; patients with chronic comorbid disease including cardiovascular, respiratory, or liver disease and diabetes; and immunosuppressed patients because of malignancy, HIV infection, or other diseases.
•Oseltamivir or zanamivir treatment should be started as soon as possible after the onset of illness in patients in at-risk groups who have uncomplicated illness caused by influenza virus infection (strong recommendation, very low quality evidence).
Recommendations for Chemoprophylaxis of H1N1
Specific recommendations regarding the use of antivirals for chemoprophylaxis of pandemic (H1N1) 2009 influenza virus infection are as follows:
•When risk for human-to-human transmission of influenza is high or low, and the probability of complications of infection is high, either because of the influenza strain or because of the baseline risk of the exposed group, use of oseltamivir or zanamivir may be considered as postexposure chemoprophylaxis for the affected community or group, for individuals in at-risk groups, or for healthcare workers (weak recommendation, moderate-quality evidence).
•Individuals in at-risk groups or healthcare personnel need not be offered antiviral chemoprophylaxis if the likelihood of complications of infection is low. This recommendation should be applied independent of risk for human-to-human transmission (weak recommendation, low-quality evidence).
For treatment of mild to moderate uncomplicated clinical presentation of infection with multiple cocirculating influenza A subtypes or viruses with different antiviral susceptibilities, patients in at-risk groups should be treated with zanamivir or oseltamivir plus M2 inhibitor (noting that amantadine should not be used in pregnant women). Otherwise-healthy patients with this presentation need not be treated.
When the clinical presentation of infection with multiple cocirculating influenza A subtypes or viruses with different antiviral susceptibilities is severe or progressive, all patients should be treated with oseltamivir plus M2 inhibitor, or zanamivir.
For treatment of mild to moderate uncomplicated clinical presentation of infection with sporadic zoonotic influenza A viruses including H5N1, the at-risk population should be treated with oseltamivir or zanamivir, and the otherwise-healthy population with oseltamivir. All patients, regardless of risk status, with severe or progressive presentation of infection with sporadic zoonotic influenza A viruses including H5N1 should be treated with oseltamivir plus an M2 inhibitor.
((News From MEDSCAPE NEWS))
Irrirtable Bowel Syndrome IBS : Short review and Rome II Criteria

Differential Diagnosis
Symptoms
The primary symptoms of IBS are abdominal pain or discomfort in association with frequent diarrhea or constipation, a change in bowel habits. There may also be urgency for bowel movements, a feeling of incomplete evacuation (tenesmus), bloating or abdominal distention. People with IBS more commonly than others have gastroesophageal reflux, symptoms relating to the genitourinary system, psychological symptoms, fibromyalgia, chronic fatigue syndrome, headache and backache.
Rome Process for Diagnosing IBS
The cardinal requirement for the diagnosis of IBS is abdominal pain. The Rome II criteria is used to diagnose IBS after a careful examination of the patient's medical history and physical abdominal examination which looks for any 'red flag' symptoms. More recently, the Rome III criteria, incorporating some changes over the previous set of criteria, have been issued. The Rome II and III efforts have integrated pediatric contents to their set of criteria.
According to the Rome II committees and the Functional Brain Gut Research Group, IBS can be diagnosed based on at least 12 weeks, which need not be consecutive, of the preceding 12 months there was abdominal discomfort or pain that had two out of three of these features:
Relieved with defecation; and/or
Onset associated with a change in frequency of stool; and/or
Onset associated with a change in form (appearance) of stool.
Symptoms that cumulatively support the diagnosis of IBS:
Abnormal stool frequency (for research purposes, "abnormal" may be defined as greater than 3 bowel movements per day and less than 3 bowel movements per week);
Abnormal stool form (lumpy/hard or loose/watery stool);
Abnormal stool passage (straining, urgency, or feeling of incomplete evacuation);
Bloating or feeling of abdominal distention.
Supportive symptoms of IBS:
A) Fewer than three bowel movements a week
B) More than three bowel movements a day
C) Hard or lumpy stools
D) Loose (mushy) or watery stools
E) Straining during a bowel movement
F) Urgency (having to rush to have a bowel movement)
G) Feeling of incomplete bowel movement
H) Passing mucus (white material) during a bowel movement
I) Abdominal fullness, bloating, or swelling
Diarrhea-predominant: At least 1 of B, D, F and none of A, C, E; or at least 2 of B, D, F and one of A or E.
Constipation-predominant: At least 1 of A, C, E and none of B, D, F; or at least 2 of A, C, E and one of B, D, F.
Red flag symptoms which are not typical of IBS:
Pain that awakens/interferes with sleep
Diarrhea that awakens/interferes with sleep
Blood in the stool (visible or occult)
Weight loss
Fever
Abnormal physical examination

Specific Virus Families causing disease in animals and plants
- Adenovirus

- Afican Swine Fever Virus

- Animal Viruses

- Arbovirus

- Arenavirus
- Arterivirus
- Astrovirus
- Bacteriophage
- Baculovirus

- Bunyavirus

- Calicivirus

- Caulimovirus

- Coronavirus
- Filovirus

- Flavivirus

- Hepadnavirus

- Herpesvirus
- Myovirus

- Nodavirus

- Orthomyxovirus

- Paramyxovirus

- Papovavirus

- Parvovirus

- Phycodnavirus

- Picornavirus

- Poxvirus
- Reovirus

- Retrovirus

- Rhabdovirus

- Togavirus
- Viroids
Swine Flu : Who Are at Risk
Which groups are at greatest risk?
Some people are more at risk than others of serious illness if they catch swine flu. They will need to start taking antivirals as soon as they are confirmed with the illness. On occasion, doctors may advise some high risk patients to take antivirals before they have symptoms if someone close to them has swine flu.
The risk profile of the virus is still being studied but it is already known that certain groups of people are particularly vulnerable. These include:
- Patients who have had drug treatment for asthma in the past three years
- Pregnant women
- People aged 65 years and older
- Children under five years old
- People with chronic lung disease
- People with chronic heart disease
- People with chronic kidney disease
- People with chronic liver disease
- People with chronic neurological disease
- People with immunosuppression (whether caused by disease or treatment)
- People with diabetes mellitus
Why are healthy people over 65 and children not a priority for the swine flu vaccine?
Healthy people aged over 65 appear to have some natural immunity to the swine flu virus. And while children are disproportionately affected by swine flu, the vast majority make a full recovery - therefore the experts do not advise that children (other than those in at-risk groups) should be vaccinated initially.
Aishwarya Rai Syndrome and Hrithic Roshan Syndrome

Taken from New O.P. Ghai, 6th edition, page number 70,
It is a syndrome, given in O.P.Ghai,( possibility, may be ask the question in some entrances, at least in state PG)
" Issues regarding body weight,general attractiveness, breast size,complexion, and acne are some of the main body image concerns for adolescent girls."
It actually comes under Body Image Syndromes.
Similarly
Hrithic roshan Syndrome for Boys
Diagnostic Criteria For Systemic Lupus Erythematosus, ACR
1. Serositis: Pleuritis (inflammation of the membrane around the lungs) or pericarditis (inflammation of the membrane around the heart); sensitivity = 56%; specificity = 86% (pleural is more sensitive; cardiac is more specific).
2. Oral ulcers (includes oral or nasopharyngeal ulcers).
3. Arthritis: nonerosive arthritis of two or more peripheral joints, with tenderness, swelling, or effusion; sensitivity = 86%; specificity = 37%.
4. Photosensitivity (exposure to ultraviolet light causes skin rash, or other symptoms of SLE flareups); sensitivity = 43%; specificity = 96%.
5. Blood—hematologic disorder—hemolytic anemia (low red blood cell count) or leukopenia (white blood cell count<4000/µl), class="mw-redirect">lymphopenia (<1500/µl) sensitivity =" 59%;" specificity ="">
6. Renal disorder: More than 0.5g per day protein in urine or cellular casts seen in urine under a microscope; sensitivity = 51%; specificity = 94%.
7. Antinuclear antibody test positive; sensitivity = 99%; specificity = 49%.
8. Immunologic disorder: Positive anti-Smith, anti-ds DNA, antiphospholipid antibody, and/or false positive serological test for syphilis; sensitivity = 85%; specificity = 93%. Presence of anti-ss DNA in 70% of cases (though also positive with rheumatic disease and healthy persons)
9. Neurologic disorder: Seizures or psychosis; sensitivity = 20%; specificity = 98%.
10. Malar rash (rash on cheeks); sensitivity = 57%; specificity = 96%.
11. Discoid rash (red, scaly patches on skin that cause scarring); sensitivity = 18%; specificity = 99%.
The mnemonic to remember the 11 symptoms is 'SOAP BRAIN MD'.
Some people, especially those with antiphospholipid syndrome, may have SLE without four criteria, and also SLE may present with features other than those listed in the criteria.
Bed Bug Bites
Bedbugs seem to possess all of the necessary prerequisites for being capable of passing diseases from one host to another, but there have been no known cases of bed bugs passing disease from host to host. There are at least twenty-seven known pathogens (some estimates are as high as forty-one) that are capable of living inside a bed bug or on its mouthparts. Extensive testing has been done in laboratory settings that also conclude that bed bugs are unlikely to pass disease from one person to another. Therefore bedbugs are less dangerous than some more common insects such as the flea. However, transmission of Chagas disease or hepatitis B might be possible in appropriate settings.
The salivary fluid injected by bed bugs typically causes the skin to become irritated and inflamed, although individuals can differ in their sensitivity. Anaphylactoid reactions produced by the injection of serum and other nonspecific proteins are observed and there is the possibility that the saliva of the bedbugs may cause anaphylactic shock in a small percentage of people. It is also possible that sustained feeding by bedbugs may lead to anemia. It is also important to watch for and treat any secondary bacterial infection.

Top 10 Epidemics of All time


| Measles | | Number 10 |
| Polio | | Number 9 |
| Yellow Fever | | Number 8 |
| AIDS | | Number 7 |
| Malaria | | Number 6 |
| Tuberculosis (TB) | | Number 5 |
| Cholera | | Number 4 |
| Plague (bubonic and Pneumonic) | | Number 3 |
| Smallpox | | Number 2 |
| Influenza or “flu” | | Number 1 |















